The Genetics of 5q Spinal Muscular Atrophy
The Genetics of 5q Spinal Muscular Atrophy
Who this is for
Many people want to learn more about the genetics that have led to Spinal Muscular Atrophy (SMA) in their immediate or extended family. They want to better understand the condition, what it means for future pregnancies and for other family members, and what genetic treatment options might be available in the future.
In this guide
This guide covers the genetics of 5q SMA which includes childhood onset SMA Types 1, 2 and 3 and adult onset SMA Type 4.
You can ask your own or your child’s clinical team to go over any of this information with you. They should be able to provide you with genetic information that applies to your individual situation.
There are other rarer forms of SMA with other genetic causes. Our information sheets about these can be found on our website here.
For more information about 5q SMA please see:
Genetic conditions are caused by alterations in our genes which prevent the gene from working properly.
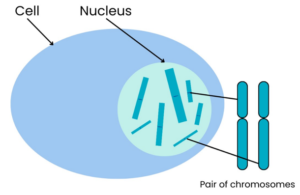
Our bodies are made up of many millions of cells. Nearly all cells have a structure called the nucleus, which contains chromosomes that contain genes.
Chromosomes are compact bundles of DNA. (See Box 1 for an explanation of DNA.)
A gene is a specific section of DNA.
Body cells have two copies of each chromosome, as we inherit one copy from each parent.
We all have 46 chromosomes in each cell in our body and these are arranged in 23 pairs.
This means we have two copies of every gene.
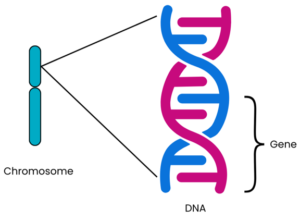
Genes are a sequence of code (called base pairs) which are read by the body to make proteins (see Box 1 for more information). Our cells need proteins for their structure, survival and to work correctly. We each have approximately 20,000 different genes making different proteins in our bodies¹‾². Each protein made by a different gene has its own unique function. The structure of the protein, and therefore its function, is determined by the order in which the base pairs are arranged in that particular gene. Usually, there are two copies of each gene on each chromosome pair: one inherited from each parent.
Sometimes a gene can contain an alteration known as a mutation. Genetic conditions occur when a mutation within a gene affects how the protein in our bodies is produced and how it works.
Box 1 – an explanation of DNA
DNA is often described as a recipe book, or a set of instructions, because it contains the information needed for a person to grow and develop.
DNA is made up of lots of nucleotides joined together. Each nucleotide contains a phosphate, a sugar and a base. The phosphate and sugar are always the same but the base varies in each nucleotide. The base can be one of four: adenine (A), guanine (G), cytosine (C), or thymine (T).
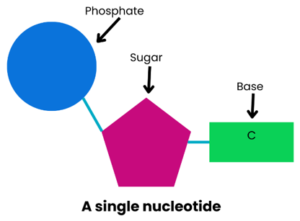
These bases pair up: A with T, C with G. The order in which these pairs of bases are arranged affects how the ‘recipe book’ information is read. The joined base pairs hold the nucleotides together in strands that twist together to form the DNA double-helix shape.

- The SMN1 gene
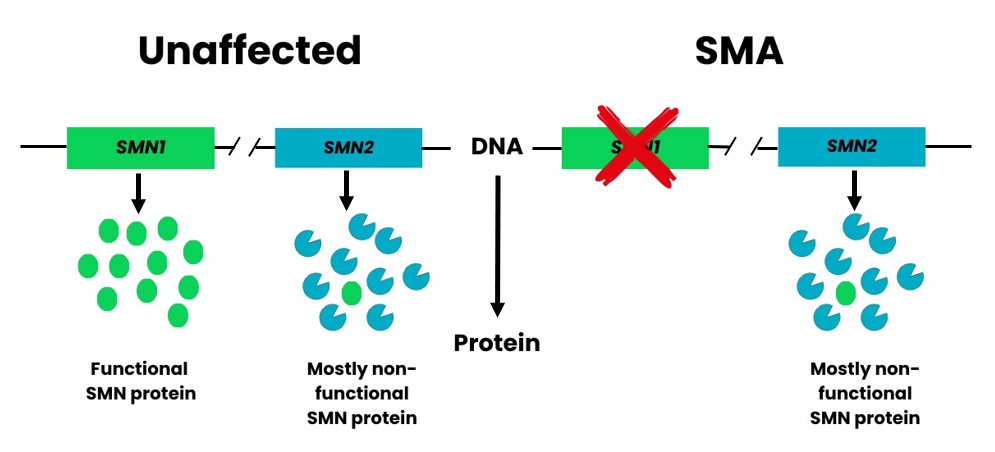
Most people have two copies of the SMN1 gene. People with 5q SMA have two copies of the SMN1 gene which do not work properly. This means they are unable to produce enough SMN protein to have healthy lower motor neurons4.
- The SMN2 gene
A second gene also has a role in producing SMN protein. This is the Survival Motor Neuron 2 (SMN2) gene, sometimes referred to as the SMA “back-up gene”.
SMN2 has an important single base (nucleotide) difference from SMN1. This causes a small section of the gene, called Exon 7, to be excluded in the majority of SMN protein that the SMN2 gene makes. It is estimated that only about 10% of the SMN protein made from SMN2 is functional5.
A deletion describes a type of mutation when a small section of DNA is missing. When part or all of a gene is missing, it can no longer make healthy protein. Instead, a shorter, often less functional (less useful) protein is made, or in some instances no protein at all.
About 95 in 100 (95%) of people with 5q SMA have a deletion of part of each of their two copies of the SMN1 gene. This is called a homozygous deletion.
The other 5 in 100 (5%) of people with SMA have a point mutation. This is when a single base (nucleotide) within the DNA is altered. Often, these people will have the more common deletion mutation in one of their copies of SMN1 and the point mutation in the other copy
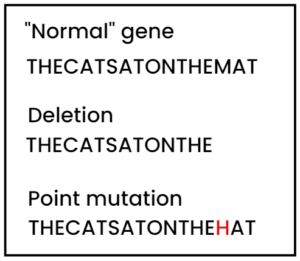
Figure 2. Deletion and Point Mutations. Taken from Skirton. H. and Patch, C. (2009) Genetics for the Health Sciences. Oxford: Scion Publishing.
People have 23 pairs of chromosomes. 22 of the pairs are non-sex chromosomes, known as autosomes, and which are found in both males and females. The 23rd pair consists of two sex chromosomes, which determine your sex. Females usually have two X chromosomes (XX), and males an X and a Y chromosome (XY).
SMA is an autosomal recessive condition. This means that the gene alteration (mutation) causing the condition is located on one of the autosomal chromosomes³, and not one of the two sex chromosomes. More specifically, for 5q SMA, the Survival Motor Neuron 1 (SMN1) gene is located on the fifth
autosomal chromosome (chromosome 5), in the region labelled ‘q’.
In an autosomal recessive condition like 5q SMA:
- a person will only have SMA if they inherit two altered copies of the SMN1 gene
- a person who carries one altered copy of the gene and one healthy copy will not have the condition but is a carrier. They do not have any symptoms, but the altered gene can be passed on to their children.
The chances of your children being carriers or having 5q SMA due to the way autosomal recessive genetic conditions are passed on will depend on whether you or your partner have 5q SMA, or are carriers. The chances stay the same for each pregnancy; having one child who has 5q SMA or is a carrier doesn’t change the chances for any further children.
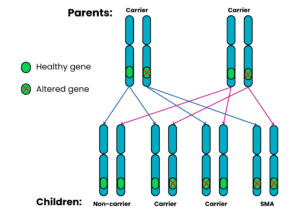
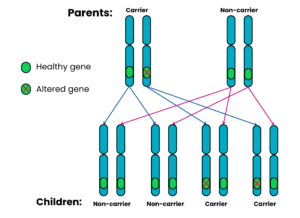
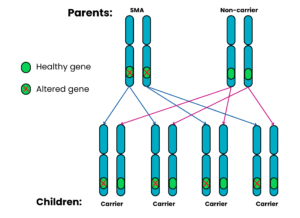
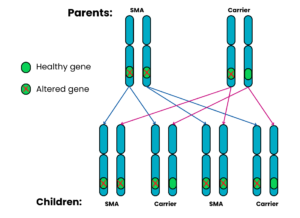
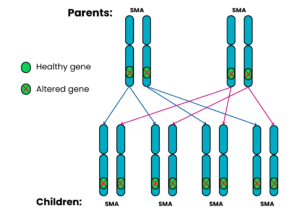
The following diagrams show what the chances are in different families.
For the purpose of the diagrams, a ‘non-carrier’ means a person who does not carry the altered gene and does not have SMA.
Autosomal recessive family 1: Both parents are carriers
For each pregnancy, the chances are:
- Child will not have SMA and will not be a carrier: 1 in 4 chance (25%)
- Child will not have SMA but will be a carrier: 2 in 4 chance (50%)
- Child will have SMA: 1 in 4 chance (25%)
Autosomal recessive family 2: One parent is a carrier, the other does not have SMA and is a non-carrier
For each pregnancy, the chances are:
- Child will have SMA: very low risk* (see below)
- Child will not have SMA and will not be a carrier: 2 in 4 chance (50%)
- Child will not have SMA but will be a carrier: 2 in 4 chance (50%)
Autosomal recessive family 3: One parent has SMA, the other does not have SMA and is a non-carrier
For each pregnancy, the chances are:
- Child will have SMA: very low risk* (see below)
- Child will not have SMA and will not be a carrier: not possible
- Child will not have SMA but will be a carrier: 4 in 4 chance (100%)
Autosomal recessive family 4: One parent has SMA, the other is a carrier
For each pregnancy, the chances are:
- Child will not have SMA and will not be a carrier: not possible
- Child will have SMA: 2 in 4 chance (50%)
- Child will not have SMA but will be a carrier: 2 in 4 chance (50%)
Autosomal recessive family 5: Both parents have SMA
For each pregnancy, the chances are:
- All the children will have SMA (100%)
Yes – 5q SMA can result from complicated, but rare, scenarios, including “de novo” mutations and “germline mosaicism”.
In most cases, mutations in SMN1 are clearly inherited from a parent who is a carrier. However, there are a very small number of people who develop 5q SMA despite standard carrier tests showing that one or both parents are not carriers with an altered SMN1 gene. This occurs in approximately 1 in 50 (2%) cases of 5q SMA. It can happen because the SMN1 mutation is new in the affected person or is not clearly present in the cells analysed in the carrier test. This situation can be caused by either a “de novo” mutation or something known as “germline mosaicism” in a parent.
- De Novo
De novo means “from the beginning” and is a type of mutation that occurs either when an individual sperm or egg is made, when a sperm fertilises an egg, or when cells are dividing after fertilisation. The most likely reason is an error in the making of the sperm or egg cell. As it occurs at this stage, the mutation will not be detected in either of the parents.
- Germline Mosaicism
Alternatively, a parent may have something known as germline mosaicism, which is when an individual produces sperm or egg cells that differ in their genetics from all the other cell types in the body of that person. If the SMN1 gene is affected in this way, the sperm or eggs of that individual can have an altered SMN1 gene, which would go undetected by the carrier test.
These rare scenarios can have implications for the chance of 5q SMA affecting a future pregnancy, and highlight the importance of having genetic counselling specific to your own circumstances.
- Silent Carriers of 5q SMA
Another scenario where someone is a carrier for SMA, but it may not be identified by standard genetic testing, is when a parent has two or more copies of SMN1 on the same chromosome. In these cases, the laboratory may not be able to detect that the person carries a deletion within the SMN1 gene on the different chromosome in the pair. However, it may be possible for the genetics laboratory to work this out, by testing other family members or by doing further testing.
Carrier testing for genetic conditions will never be 100% sensitive, but the laboratory and your genetics team can discuss any limitations of the testing with you. They will also try to ensure the testing for your family is as accurate as possible.
- Genetic counselling
Genetic counselling is with a healthcare professional who has expert training in genetics. They’ll aim to explain results from your genetic testing in an easily understandable way, and answer any questions you might have about the genetic aspects of the diagnosis.
Common issues to discuss in genetic counselling might include implications or options for a future pregnancy, and whether there is a need to discuss the diagnosis with other family members who might wish to seek genetic counselling.
Q. We do not have SMA ourselves, but have had one child with SMA. How can we find out if our next child will also have SMA?
A: It is most likely that you and your partner are both carriers of the gene alteration that causes 5q SMA. A referral to a Clinical Genetics Service for genetic counselling is important so that you can get advice specific to your own circumstances and consider your future options (see below). If you have another pregnancy together, the chance that your next child will have 5q SMA is likely to be 1 in 4 (25%), as shown in the Family 1 diagram. The copy of each gene inherited from each parent is random and cannot be predicted. Some couples who are both carriers decide to take that chance, while others want to consider alternative options when having children.
Our information on Family Planning For Couples Affected By 5q SMA tells you more about these options.
You can also discuss what is possible with the healthcare professionals involved who should be able to help you make this very personal decision.
Q. I am a carrier, should I suggest that other family members get tested?
A: As genes are inherited from parents, and passed on from generation to generation, you share many of your genes with members of your extended family. It is therefore possible that your blood relations may also be carriers of the same gene alteration. You might want to tell your relations about this so that they have the option of asking for genetic counselling to obtain more information, and to have carrier testing if they wish to do so. This can be particularly relevant if they are considering a pregnancy in the future.
Q: My partner is a carrier of SMA and we are thinking of having children. Where can I get tested to see if I am a carrier too?
A: Ask your G.P. to refer you to your regional clinical genetics centre. The main genetics clinics are usually in large cities, but outreach clinics may be held in other smaller hospitals across the region. You may also be offered a phone or virtual appointment, to avoid the need to travel to a clinic appointment.
Q: In a family with 5q SMA, who will be able to have genetic testing?
A: Staff at your regional genetics centre can give you specific advice about who might need to be tested. Close family members will be seen first to identify who might be carriers. The staff might work with you to draw a family tree.
Q: There is a history of 5q SMA in my family. When should my partner and I have genetic testing?
A: Genetic counselling before pregnancy will give you and your partner more time to think about genetic testing and the possibly difficult decisions this can raise. But, you can still seek genetic counselling if you are already pregnant – just make sure to say you are and ask to be seen urgently.
Q: What is the waiting time for a genetics appointment?
A: You will usually be offered an appointment within 18 weeks. However, you will be seen much sooner (usually within a few days) if you are currently pregnant and have a family history of SMA.
Q: A member of my family has been diagnosed with 5q SMA. I am pregnant and I do not know if I am a carrier. How do I get a quick referral to genetic services?
A: Contact your midwife or G.P. to ask for an urgent genetic counselling referral. If this is not possible you can contact your local genetic service directly (there is a list of centres on the Genetic Alliance UK website). You and your partner may be offered testing.
Q: I have no family history of 5q SMA, can I still be tested?
A: Genetic testing is not usually available on the NHS to people with no personal family history or connection to 5q SMA.
Q: Can I have a genetic test for 5q SMA without having genetic counselling?
A: This is generally not possible via the NHS. Genetic counselling will give you the most up-to-date and accurate information enabling you to make informed choices about the options available to you.
Q: How long will it take to get the results of a genetic test for 5q SMA?
A: The test result is usually available within 2 – 4 weeks, but can sometimes take longer. Testing can be completed more urgently in certain situations (for example, in pregnancy or a very unwell baby).
Q: I have been tested for 5q SMA and the test has come back negative but my consultant still thinks I have SMA. Is this possible?
A: In a small number of cases the genetic basis is more complex and further genetic and / or other testing may be necessary. Your doctor will advise you depending on your symptoms and the tests you have had so far.
Q: My son has SMA symptoms but the test has come back negative. Is it possible that he has SMA?
A: Routine testing for SMA will confirm the diagnosis in the majority of people but sometimes further genetic and / or other testing may be needed. Your doctor will advise you depending on your son’s symptoms and the tests he has had so far. This may include investigations for other conditions that can present in a similar way to SMA.
Q: My daughter has been diagnosed with 5q SMA. I am worried that her brother and sister might develop 5q SMA too. Should they be tested?
A: It is important for you to discuss this with the healthcare professionals involved and your family. Your decision may be influenced by the Type of SMA your daughter has and whether you already have worries about the health of your other children.
Q: My sister’s son has been diagnosed with 5q SMA. I have a 4-year-old daughter and I am worried that she might develop SMA too. Should I have her tested?
A: You could request carrier testing at a genetic centre to see whether you are a carrier of 5q SMA. Once you have your own result you can discuss with your healthcare professionals and your family whether to test your daughter. Genetic centres do not always offer carrier testing in childhood as it removes the child’s right to make an informed decision when they are older.
Q. For the last 20 years or so, I have had weakness and difficulties and more recently my mobility has deteriorated further. Our grandchild has recently been diagnosed with SMA Type 3 and I now wonder if I might have SMA too. Can I request genetic testing?
A: There is a possibility that you might have SMA. You can ask your G.P. to refer you to a neurologist, who can review your symptoms. Your clinical signs and family history will be reviewed, and you may be offered genetic testing for SMA. They may also advise on whether they think the weakness and mobility issues are being caused by something other than SMA.
Q. We have SMA on my side of our extended family, but I have not had carrier testing. My children are now young adults and I have been told by my genetics centre that I do not need carrier testing now, as I am not planning to have any more children myself. What do you advise about this?
A: If a patient is referred to clinical genetics with a family history of SMA, the genetics team would review the family tree and decide which relatives would benefit from genetic testing. They will discuss this decision with you and may suggest that other relatives are tested before you have testing yourself.
Q: Two generations ago, my grandma’s first child died. From what I’ve read about SMA, I think the child might have had SMA Type 1. There was no genetic confirmation, so I understand I may not be eligible for NHS carrier testing. Can I have testing privately?
A: It is always preferable to use NHS services where possible, as this ensure high quality testing by qualified scientists and medics and we are not able to recommend any specific private health services in the UK. If the only option is private testing, to be assured of quality, private providers should be able to match this level of registration / accreditation:
- NHS labs are accredited by UKAS. Their website lists all of the molecular genetic labs accredited in this way.
- NHS doctors are registered on the GMC register.
- NHS genetic counsellors are registered with:
Genetics and Genetic Testing:
- Genetic Alliance UK
Tel: 0207 704 3141
Clinical trials information:
- Our website page: How Clinical Trials Work
- Current clinical trials in SMA can be searched for on the clinicaltrials.gov website
- The UK SMA Patient Registry
For the latest developments with drug treatments, the science behind them, and what clinical trials and other research is going on, please click see this section of our website.
To receive our monthly E-newsletter, sign up for mailings on our website, here.
- International Human Genome Sequencing Consortium (2004) ‘Finishing the euchromatic sequence of the human genome’, Nature, 431, pp. 931-945.
- Pennisi, E. (2012) ‘ENCODE project writes eulogy for junk DNA’, Science, 337(6099), pp. 1159-1161.
- Lefebvre, S., Bürglen, L., Reboullet, S., Clermont, O., Burlet, P., Viollet, L., Benichou, B., Cruaud, C., Millasseau, P., Zeviani, M., Le Paslier, D., Frézal, J., Cohen, D., Weissenbach, J., Munnich, A., and Melki, J. (1995) ‘Identification and characterization of a spinal muscular atrophy-determining gene’, Cell, 80(1), pp. 155-165.
- Verhaart IEC, Robertson A, Wilson IJ, Aartsma-Rus A, Cameron S, Jones CC, Cook SF, Lochmüller H (2017) Prevalence, incidence and carrier frequency of 5q–linked spinal muscular atrophy –a literature review. Orphanet J Rare Dis 12: 124.
- Ruggiu, M., McGovern, V.L., Lotti, F., Saieva, L., Li, D.K., Kariya, S., Monani, U.R., Burghes, A.H. and Pellizzoni, L. (2012) ‘A role for SMN exon 7 splicing in the selective vulnerability of motor neurons in spinal muscular atrophy’, Molecular and Cellular Biology, 32(1), pp. 126-138.
- Burghes, A.H. and Beattie, C.E. (2009) ‘Spinal muscular atrophy: why do low levels of survival motor neuron protein make motor neurons sick?’ Nature Reviews Neuroscience, 10, pp. 597-609.
- Butchbach M (2016) ‘Copy Number Variations in the Survival Motor Neuron Genes: Implications for Spinal Muscular Atrophy and Other Neurogenerative Diseases’, Frontiers in Molecular Neurosciences, Volume 3. Article 7.
- Lefebvre S, Burlet P, Liu Q, Bertrandy S, Clermont O, Munnich A, Dreyfuss G, Melki J (1997). Correlation between severity and SMN protein level in spinal muscular atrophy. Nat Genet 16: 265–269.
- Mailman MD, Heinz JW, Papp AC, Snyder PJ, Sedra MS, Wirth B, Burghes AHM, Prior TW (2002). Molecular analysis of spinal muscular atrophy and modification of the phenotype by SMN2. Genet Med 4: 20–26.
- Eugenio Mercuri, et al., Diagnosis and management of spinal muscular atrophy: Part 1 Recommendations for diagnosis, rehabilitation, orthopedic and nutritional care. Neuromuscular Disorders (2017), doi: 10.1016/j.nmd.2017.11.005 Available at: https://www.sciencedirect.com/science/article/pii/S0960896617312841?via%3Dihub (last accessed 10th August 2022)
 Version 5
Version 5
Author: SMA UK Information Production Team
Last updated: December 2023
Next full review due: May 2026
Links last checked: March 2024
The information provided in this guide, on our website, and through links to other websites, is designed to complement not be a substitute for clinical and professional care and advice.
For more detail about how we produce our information, please see these pages.
If you have any feedback about this information, please do let us know at: information@smauk.org.uk